So, About Screens…
Screens are everywhere. Most kids around the country now access their reading assignments, quizzes and tests, and other school materials via tablets and iPads. Speech therapists, daycares, and parents use speech and language development apps. Kids have video chats with long-distance relatives and friends–sometimes even strangers online. Ms. Rachel, TikTok, Danny Go, Call of Duty, YouTube Kids, texting, insta, snap, X. Electronics have take over everyone’s lives, and even the youngest of kids aren’t immune to the endless doom scroll.
It’s common for all parents to wonder how much is too much, what kinds of content to allow or restrict, and how to balance supervision with enabling kids with good habits even when they’re not being watched. For parents and caregivers of neurodivergent children, screens can feel like a double-edged sword: powerful tools for learning, communication, and even connection, but also potential sources of overstimulation, sleep disruption, or distraction from other learning, play, and live social interactions.
So. Let’s talk about it.
What Are the Official Guidelines?
The American Academy of Pediatrics (AAP) recommends avoiding or minimizing screen time for infants and emphasizes co-viewing and high-quality content for toddlers and preschoolers. A main reason for this is the hands-on learning that babies and toddlers need to strengthen mental relationships with the information around them. While digital media can help with language development, it does not replace real-world social practice and feedback. “Feedback” can often make people think of critiques and coaching, but we give our kids feedback constantly–head nods, praise, smiles, furrowed brows, copying them–that shapes how they interact with others and their environment moving forward.
Similarly, The World Health Organization (WHO) recommends minimal to no sedentary screen time for children under 2, and for 2- to 4-year-olds limits sedentary screen time to no more than 1 hour per day, with less time being better. They emphasize replacing screen time with active play and caregiver interaction for the same reasons as given above.
Some people continue to make claims that screen time from an early age or excessive childhood screentime cause autism and contribute to the ever-growing prevalence of autism in the United States. A recent systematic review and meta-analysis concluded that, while some associations exist, the evidence is mixed, effect sizes are generally small, and most studies are correlational–in other words, high amounts of screen exposure often appears alongside autism, but we can’t say definitively that one causes the other.
Importantly, screens are also being used successfully as intervention tools for autistic children. Evidence supports the use of augmentative and alternative communication (AAC) apps, video-modeling, and telehealth-delivered therapies to improve communication and social skills for many autistic children. These are not the same as passive screen time, like YouTube videos, but instead are structured tools used with a therapeutic goal.
How to Make Screen Work For You, Not Against You
The guidelines above are baseline public-health recommendations, aimed at typically developing populations, and are intentionally conservative. It doesn’t mean that you’re a bad parent if you provide more than an hour or that your child will fail to thrive. It’s useful to overlay these guidelines with individualized considerations: communication needs, sensory profile, sleep, therapy goals, and what’s actually working for your child. Screens can be neutral, harmful, or helpful depending on how they’re used. Like most things, context matters.
We can approach screen times the way many of us do junk food, staying up late, and playdates: with a plan for moderation, safety, and as enhancements rather than harmful habits.
Purpose
Before handing over a device, ask: What is this screen time for?
- Entertainment/relaxation? Use short, predictable videos and set (and keep) an end time.
- Communication (AAC)? Make it part of a daily routine and pair it with adult modeling.
- Learning/therapy? Coordinate with the child’s therapist(s) so the app supports skill goals.
Purposeful, goal-driven screen use is more likely to produce benefit and less likely to displace therapy or real-world practice.
Interactive > Passive
Apps that let a child communicate (AAC), practice social scripts, or receive video modeling can produce measurable gains. If a clinician recommended an app, continue to use it as prescribed and track progress.
Educational games, like tracing, identifying shapes/letter/numbers, matching, and applying other academic, social, or safety skills tend to require more engagement compared to YouTube, YouTube Kids, and TikTok. While there is educational content on all of these platforms, there aren’t as many opportunities to practice what is learned and receive feedback, as described above.
You can even build more interactive opportunities into passive viewing. Do the dances and the songs with your child to their favorite videos. Narrate what’s going on. Ask your school-age kiddo questions about the craft or video game playthrough they just watched. For the teens who like to prove they know everything (I say tongue-in-cheek), ask a dumb question and allow them to break things down for you. All of these provide those live, in-person interactions that shape social skills and help to process all that visual and audio information.
Structure
Many children, especially those who are neurodivergent, thrive on routine. Use visual schedules, timers, and clear transitional warnings (“Five more minutes of video, then we’ll put it away and go outside”). Predictable limits reduce meltdowns and power struggles. See our recent blog post on making transitions easier for more guidance if this is an area where your child seems to have a harder time.
LOADING: OVERSTIMULATION 95%…
Screens, with their bright flashing lights, intense colors, and loud or repetitive noises, can overstimulate any child. If a child becomes more irritable, zones out for long periods, experiences sleep disruption, or shows increased repetitive behaviors after screen sessions, shorten or change the content.
Moving forward, as patterns emerge (for example, most cartoons are fine but this specific cartoon leads to unsafe behaviors), try to hide or at least limit access to content that triggers unwanted behaviors. Your child might be upset initially to only have 1 episode of Matt the Danger Cat (made up) before moving on to something calmer, but if it means he isn’t trying to climb and jump off the bookshelves anymore, it’s worth it.
Goodnight, Tablet
Avoid screens (especially fast-paced games or videos) in the hour before bed. Blue-light and high arousal interfere with falling asleep—this is true for all kids, and autistic children often have more fragile sleep to begin with.
What Next?
There isn’t one “right” rule for every autistic child. Instead of reading this as a prescription, read it as a flexible tool that grow and change with your child and your family’s needs over time. Aim for intentional screen use: choose tools that help your child communicate or learn, scaffold those moments with adults, protect sleep and play, and watch how your child responds. When in doubt, collaborate with clinicians, who can help turn technology into a bridge rather than a barrier.
As you put the above into practice, start with a short audit for a week. What apps? how long? when? and what happens before/after? That data helps you make targeted changes. From that information, pick one change to start: enforce a no-screens-1-hour-before-bed rule, switch evening screens to a calm video with adult co-viewing, or replace one daily screen block with a sensory play activity. Small, consistent changes beat big, unsustainable rules.
If consistency does not lead to the changes you’re looking for, talk to your child’s providers. If you suspect screen use is linked to speech delays, sleep loss, reduced social engagement, or increased restriction of interests, your child’s SLP, pediatrician, or behavior analyst can help create a plan targeted to their needs.
by Britt Bolton, owner/lead BCBA
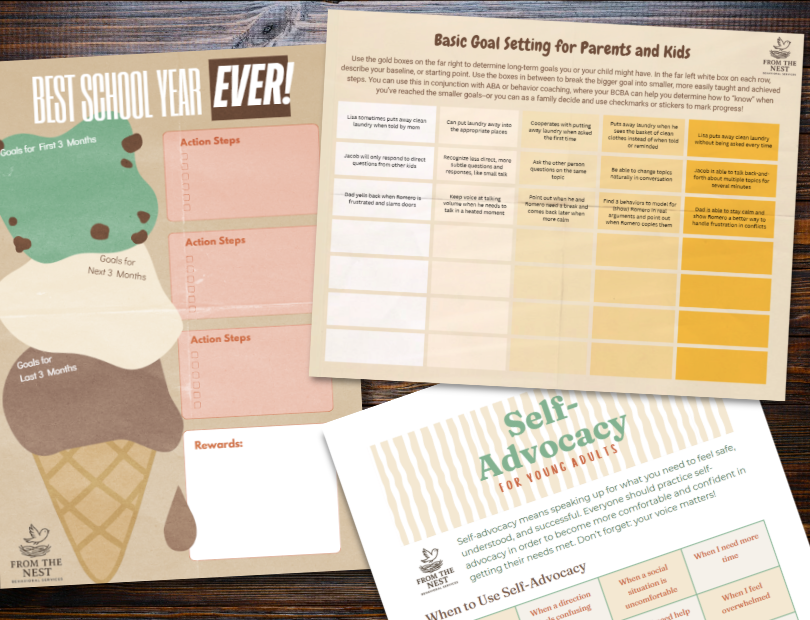
Look at our FREE Printable Resources page for routine visual supports, checklists, goal-setting worksheets, teen and young adult guides to jobs and self-advocacy, and more!
